For nearly half a million Tennesseans, chronic obstructive pulmonary disease (COPD) is a part of everyday life. Yet few of us know how to spot the signs of a COPD flare up before things get serious.
WellTuned spoke with Dr. Ian Bushell, a family medicine physician and medical director for BlueCross BlueShield of Tennessee, to find out what we need to know.
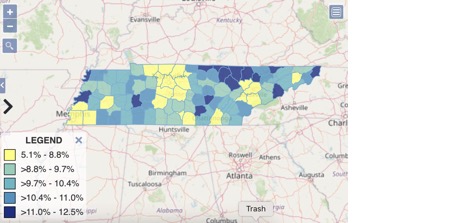
Prevalence of COPD in Tennessee by county (2019)
What is a COPD flare up or exacerbation?
Dr. Bushell: COPD, also known as emphysema or chronic bronchitis, is a medical condition in which the lungs have become damaged. Specifically, they become stiffer. When this happens, your lungs are unable to move as much air, which causes you to experience:
- Shortness of breath
- Tiredness, and
- Frequent coughing.
While COPD has no cure, there are medicines to help manage it. But, the shortness of breath and coughing can get worse for a period of time — think days, not weeks — and that is what we call a “flare up” or “exacerbation.”
What causes a COPD flare up?
Dr. Bushell: COPD flare ups have many causes, but the most common are:
- Smoking
- Exposure to smoke or other pollutants
- Stopping your medications or reducing your doses without physician instruction
- Infections (viral, bacterial or fungal)
What are the warning signs?
Dr. Bushell: The biggest warning sign of a COPD flare up is a noticeable worsening of symptoms. You’ll be more tired, more short-of-breath and/or have a worsening cough as the flare up begins.
What should you do if you notice signs of a COPD flare up?
Dr. Bushell: As soon as you notice “something different” with your chronic condition, reach out to your provider for guidance. Ideally, you should have a written plan for flare ups that you create with your provider during a visit while your condition is stable. The plan should include what to look for, what to do and when to call for help. This plan can empower you to act early. And it can help you prevent worsening of the flare up and decrease the possibility that you’ll need to be hospitalized.
Remember: flare ups will happen. It’s an expected part of having the disease. So having a plan to manage them is crucial.
What are the consequences if you have a COPD flare up?
Dr. Bushell: Flare ups vary in severity. Some can be managed at home. Others are serious enough to require hospitalization and the use of a ventilator. And, unfortunately, some may even be fatal.
However, as I said, flare ups will happen. And you can minimize your chance of having one by:
- Taking your daily maintenance medications as directed
- Not smoking
- Participating in lung rehab (pulmonary rehab)
- Staying immunized, and
- Avoiding people who are sick.
6 tips for taking your medication (and why it matters)
How are COPD flare ups treated?
Dr. Bushell: Flare ups are treated with a combination of medications that will include the following:
- Oxygen
- Antivirals and/or antibiotics and/or antifungals
- Inhalers and/or nebulizers (a powered inhaler that turns liquid medicine into mist)
- Steroids
How can you tell the difference between a “bad day” and an exacerbation?
Dr. Bushell: The biggest sign is an increase in the severity of your symptoms. You can also monitor your oxygen levels at home with an inexpensive device called a pulse oximeter — the same kind your doctor uses during visits.

To use a pulse oximeter:
- Check your oxygen levels when they are at their baseline, or usual level of functioning.
- When you start to feel different or think you may be having a “bad day,” check your oxygen level.
- If your device shows your oxygen level (O2 sat) is lower than your baseline, you’ll know it’s time to consult your care plan and/or contact your provider.
Any other advice for people who have COPD?
Dr. Bushell: Whenever you’re concerned, call your provider. Don’t be shy, don’t be afraid, don’t be too proud or embarrassed — even if you’ve stopped taking your medication or think you’ve “done something wrong.”
We understand! We won’t be mad. Things happen all the time, for lots of different reasons. We want to help you! The sooner you call, the sooner we can help and hopefully make your problem go away.
5 proactive steps for managing COPD
Dr. Bushell: COPD is a chronic problem, but it can be managed well so that it has less of an impact on your quality and length of life.
- Please stop smoking.
- Get immunized against flu, pneumonia and COVID.
- Go to “lung rehab.”
It really does help to prevent hospitalizations, and you’ll feel more energetic. - Take your medications.
If you can’t for any reason (side effects, expense, routine), please let your provider know so they can adjust them. There are other options! - Find a provider you like and trust to help you.
Dr. Bushell: If you don’t feel comfortable with the provider you have now, find another. If you need help and you’re a BlueCross BlueShield of Tennessee member, check our app or call us at 800-565-9140. Follow this advice and you can get back to chasing the kids, grandkids, dogs, fish, birds, deer, golf balls — or whatever you love to do.
More about COPD from WellTuned
- What is COPD? A guide + tips to manage it
- 5 breathing exercises for people with COPD
- Travel checklist: Asthma and COPD
Get more information about specific health terms, topics and conditions to better manage your health on bcbst.com. BlueCross BlueShield of Tennessee members can access wellness-related discounts on fitness products, gym memberships, healthy eating and more through Blue365®. BCBST members can also find tools and resources to help improve health and well-being by logging into BlueAccess and going to the Managing Your Health tab.